FAQ
-
Midwifery care is rooted in time, presence, and relationship. Our visits are typically 60 minutes, giving space for your questions and for us to truly know you, your baby, and your family. We provide the same labs, ultrasounds, and procedures you’d expect elsewhere—but with shared decision-making at the core.
We believe you are the ultimate authority on your body and your baby. Our role is to offer guidance, evidence-based information, and resources, while honoring your choices and supporting your journey with humility and respect.
-
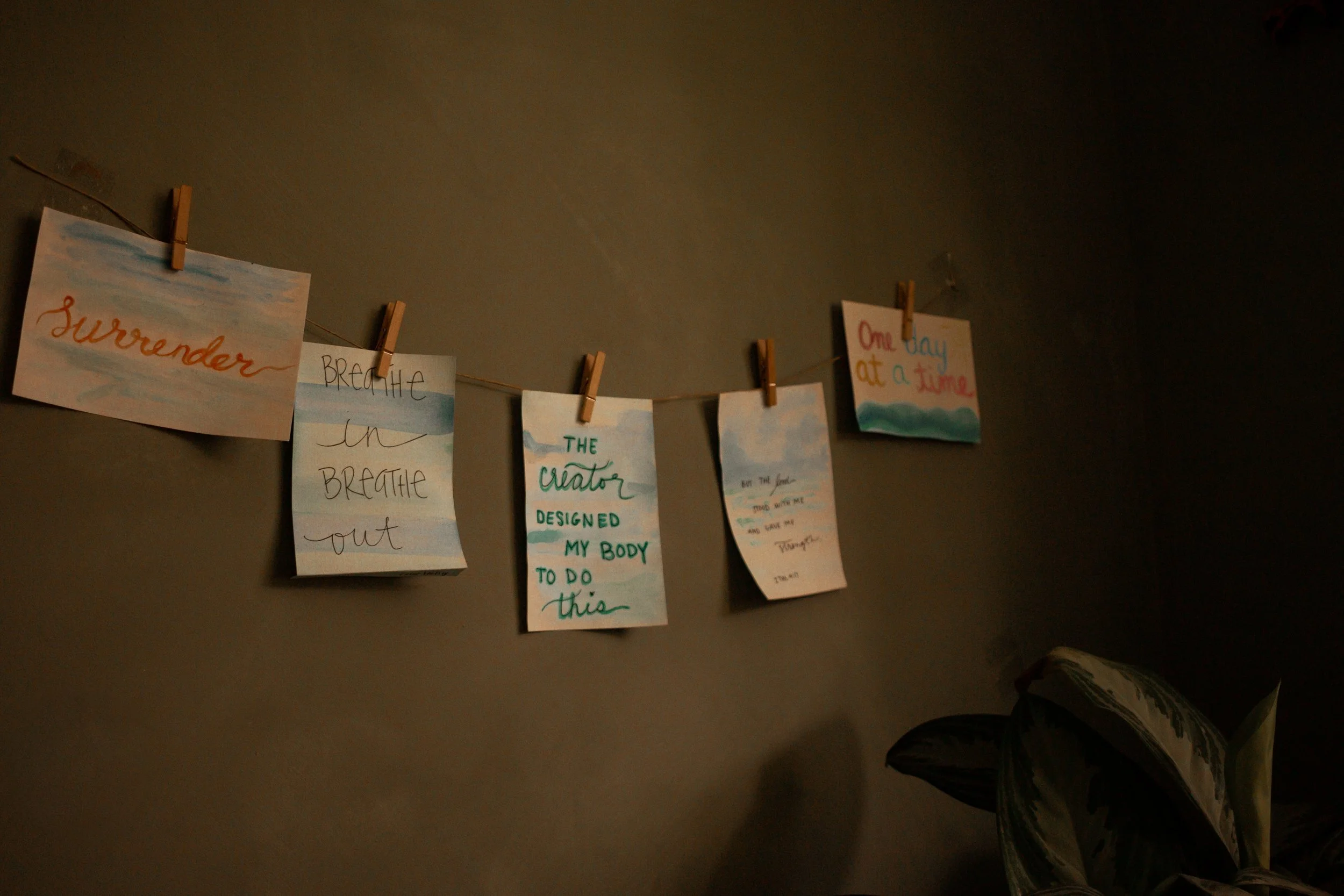
At Full Circle, we believe birth is a sacred rite of passage—an unfolding of innate wisdom that belongs to each woman. Birth is not a medical event to be managed, but a powerful, transformative journey that calls forth courage, trust, and love.
We honor the body’s natural intelligence, creating space for undisturbed birth whenever possible, while holding the skill and tools to respond when needed. Informed choice and shared decision-making are the heart of our care, for you are the final authority on your body and your baby.
Birth is also a deeply spiritual experience, connecting families to their ancestors, to the mystery of life, and to the sacredness of bringing forth new generations. We tend to the physical, emotional, and spiritual dimensions of birth, weaving ancient traditions with evidence-based care.
Our role is to safeguard the birthing space with gentleness and respect—protecting intimacy, love, and safety—while leaving room for the ineffable magic that only birth can bring.
-
Yes. In the United States and especially at Full Circle Midwifery, we believe in sharing about all of the kinds of midwives so you know how to find the one that will best serve you. Please ask the midwives you interview about their title and experience.
Traditional Midwife: Usually this type of midwife is unlicensed, has been taught midwifery through apprenticeship, was called to this work through her community, and does not carry medications, is not certified by a governing body, and truly has full allegiance to the woman and family they serve along with their own designed boundaries. In some states, these midwives are illegal or can be fined, imprisoned, or required to cease practice. This midwife can be called many names; Birthkeeper, Midwife, Traditional Midwife, Birth Attendant.
Certified Professional Midwife (CPM): This is a national certifying credential that shows that this midwife has “proven” their experience by attending approximately 100 births as a student, passed a national board exam, and maintains certain continuing education. CPMs practice in home birth or birth center practices and similar to transitional midwives, are designed to support low risk, healthy, physiologic birth outside of the hospital. There are 2 pathways to becoming a CPM. One is the performance evaluation process that follows the traditional apprenticeship model and the other is by graduating from a midwifery education accreditation council school with a degree. Both of these pathways must still pass the national exam and attend required clinical skill experiences. In some states only midwives who graduated from a MEAC school and passed the national board exam can become licensed.
Licensed Midwife(LM): Midwives in states where licensure exists are usually required to become a CPM prior to licensure. Licensure can be good and bad. A state where licensure exists allows the midwife to carry and administer life saving medications to manage complications and stay out of the hospital. An example can be IV fluids for dehydration in labor or to replace fluid volume after postpartum. On the contrary, licensed midwives are required to practice within the state’s regulatory boundaries and that can mean they can or cannot serve certain births or experiences.
Certified Nurse Midwives(CNM): Nurse Midwives are nurses first, followed by a masters in midwifery. These midwives primarily work in hospitals and serve women and birthing folks who are low risk but may want an induction, epidural, or medically focused birth experience. They are also trained in natural birth and in some states work in homes.
In the state of Florida, home birth midwives must be licensed and hold the LM credential to practice legally at home.
Estee is a licensed midwife, certified professional midwife, graduated from a MEAC college and was trained by CPMs, licensed midwives, CNMs, traditional birth attendants and OBs throughout her education journey.
-
The majority of people are considered low-risk and a good candidate for out-of-hospital birth. To learn more about the safety of birthing out of the hospital, check out this research study conducted by the Midwives Alliance of North America (MANA), which confirms the safety for low-risk families who choose to birth at home with a Midwife. Study after Study show home birth to be safe with less intervention than our hospital birth system.
-
Yes, but for reimbursement purposes only.
Every policy has different benefits and different pay schedules, so we collect our fees upfront, then we refer you to a medical biller to determine your specific insurance benefits and submitting a claim for the best possible reimbursement after your birth.As fully licensed and insured medical providers, you are likely to have our services applied to your deductible at minimum. To find out what your insurance plan will cover you can call your insurance representative and ask what your coverage is for an out of network provider providing home birth services and midwifery care.
And here's some good news: Florida statutes require that "any policy of health insurance which provides coverage for maternity care must also cover the services of certified nurse-midwives and midwives licensed pursuant to chapter 467, and the services of birth centers licensed under ss. 383.30-383.332." This includes our midwives, who are licensed under chapter 467.Healthshare plans, such as Samaritain, Christian Health Share and Zion, cover midwifery services extremely well! Check them out!!
-
Complete blood count (CBC): Evaluates the cells that circulate in your blood, like iron and platelets.
Blood type and Rh factor: Determines your blood type and Rh factor (negative or positive)
Antibody screen: Tests for antibodies that attack red blood cells
Rubella Antibody titer: Screens for German Measles
Urinalysis: Evaluates components of the urine
Pap smear: Screens for cervical cancer
Genetic screening: Screens for fetal chromosomal abnormalities and neural tube defects
Carrier screening: Screens for maternal chromosomal abnormalities
HIV, Syphilis and Hepatitis B&C screening: Standard sexually transmitted infection (STI) screening
Gonorrhea and Chlamydia cultures: Screens for gonorrhea and chlamydia
Urine Culture: Screens for bacteria in the urine
Glucose screening: screening for Gestational Diabetes Mellitus
Thyroid and hormone testing: Screens the thyroid hormones, as well as additional hormones, if necessary.
Vitamin D: Evaluates Vitamin D levels
Vaginal Microbiome: Candida, BV, Trichomoniasis, etc.
Group beta streptococcus culture: Screens for presence of vaginal/rectal GBS
Unity Genetic screening (includes fetal sex, blood type, and genetic profile)
SpeakPeek Gender Blood Test
-
Full Circle Midwifery brings all medical equipment and labor support tools. This includes a professional birth pool, birthing stool, resuscitation equipment, medications, herbs, vitals, etc.
We require the purchase of a water birth kit, if using our professional birth pool, which we have already compiled for you. We ask that this kit is purchased and delivered before our birth prep visit at 37 weeks. In addition to the water birth kit, we recommend comfort items, towels, baby blankets, a bowl, and snacks that you would normally desire.
-
The foundation of prenatal care is preventative care. We support you to make the healthiest and best choices possible to help keep your pregnancy low-risk. Additionally, we recommend standard of care lab tests and a mid-pregnancy (anatomy scan) ultrasound. We monitor the baby's heartbeat and growth throughout the pregnancy. We monitor your blood-pressure and other vital signs at every visit. Because our prenatal care is based on relationship building and listening; we are often able to catch issues before they become major problems. We also believe that trust and intuition is a huge part of care. Talk with your midwife when you have concerns!
We recognize that pregnancy and birth are unpredictable and stay vigilant to any developing problems or concerns. If additional tests or consultations are needed, we have refer to other providers, imaging centers and labs.
-
During labor the midwives will monitor the baby's heartbeat frequently and discreetly. We work to keep you hydrated, fed, and rested while also checking vital signs regularly. We have a midwife and trained birth assistant, second midwife, or student at every birth. We follow our carefully researched and frequently re-evaluated protocols and practice guidelines to make sure you stay low-risk and safe for out of hospital birth. These are available upon request.
Due to having low-risk clients with healthy, low-risk pregnancies, our transfer rate is very low (5%-10%) . We are trained to identify risk factors, manage complications, or transfer to the hospital before complications become true emergencies. We carry medications such as pitocin, IV fluids, oxygen, and resuscitation equipment that allow us to manage complications at home. As a maternity healthcare provider in the state of Florida, we also train and certify in Neonatal Resuscitation and CPR every 2 years.
During your care we discuss the reasons why we might transfer to the hospital and what happens during a transfer. We have relationships with our community hospitals and facilitate a smooth transfer of care in the small percentage of births where it might be necessary.
Lastly however, we cannot guarantee any outcome. No one can. Hospitals have stillbirths and bad outcomes too. The importance really relies on your radical self responsibility to choose the right thing for you and your family every step of the way. Your midwife is there to protect safe birth by knowing signs that it’s going off track and work with you to give you the best possible experience and outcome, but nor we nor any healthcare provider is responsible for it.
-
One of the benefits about having a midwife for your unmedicated birth is that we have helped hundreds of people do this. We have trust in you, your body and your baby, and we have skills to help. If there is one thing we know, it is that you can cope with the discomfort of normal labor. We do ask that all first time home birthers take childbirth education class and or hire a doula so that you are more prepared and confident.
Women have been doing this since the beginning of time. We find that the “mind over matter” philosophy really does ring true. The mental state, ability to relax and or overcome is greater than the physical sensation. We truly believe your body was meant for birth, and support the physiology while breaking into the psychology that may get in the way.
Your midwife also will deliver the birth pool to your home at 36 weeks. We LOVE “aquadurals” and encourage using water as a coping tool. Additionally, we bring birth balls, peanut balls, TENS units, Birth Slings, and our heart and hands to fully support you.
Lastly, we always encourage hiring a doula. They are professionals for supporting the physical and emotional “labor” of birth. Doulas and Midwives go together like Peanut Butter and Jelly!
-
Yes, it is legal for licensed midwives to offer VBAC at home in the state of Florida. We will schedule a consultation between you and an OB to review your history and the details of your c-section, assess your current pregnancy, and discuss the risks and benefits of VBAC.
Good prenatal care, adequate nutrition, and mental/emotional/spiritual preparation for labor and birth will help you prepare for your VBAC.
I recommend that all mothers, but especially VBAC mothers, seek out a supportive community of other pregnant women. There are other woman walking the same path, connect!
Find your local International Cesarean Awareness Network (ICAN) chapter! They do wonderful work through education, providing support for cesarean recovery, and promoting Vaginal Birth After Cesarean (VBAC).
-
The midwifery model of care highly focuses on preventative measures, which means transfer rates are usually low. If higher level of care is needed during the pregnancy this may be temporary, like a consultation, or permanent like being risked out of care for a medical reason. In the event of a transfer during labor, a midwife will accompany you to the hospital until delivery as your doula (even if you already have one) and complete all standard postpartum visits.
Sometimes, we need the hospital, and it’s important to recognize that need before it becomes emergent. Full Circle has a very low transfer rate on nearly 5%-10% of all births, which is similar to the national average of 10%. This means we don’t just transfer for no reason and sabotage your birth, and we also don’t put you or your baby at unnecessary risk.
It’s also important to note that the number 1 reason for transfer is not a medical emergency, or even pain relief… It’s exhaustion. So please listen to your midwife when we ask you to rest, hydrate, and eat in early labor. It’s a marathon, not a sprint.
A member of your birth team will always transfer in with you and remain until you both are stable.
-
Absolutely! We take transfers as far as the third trimester. However these is not a “late to care” discount. We often find that the energy it takes to build a relationship in such little time is just as much as a full pregnancy with our care.
Please text us to schedule a phone consultation to discuss details.
-
Full Circle books up quickly. As soon as you know you are pregnant and looking for a home birth, start your consultation and reserve your spot.
We love to see you starting in the first trimester, specifically by your 12th week gestation. This will give us plenty of time to build a trusting relationship. If you are currently being seen by another practice, we will facilitate transfer of records and can establish you into even into the third trimester.
However, the earlier the better as evidence shows that the midwifery model of care prenatally reduces poor outcomes, inductions, gestational diabetes, preeclampsia, cesareans, and poor birth experiences.
-
Yes! We encourage it. Your uterus is a muscle, it would be a disservice to not allow you to refuel as you work hard to birth your baby.
At your birthing time visit, we will help you gather snacks and hydration for labor.
-
We are fully trained and experienced in laceration repair and carry all legal medication to make the experience more comfortable. In the extremely rare scenario you tear more extensively, we will accompany you to the hospital for the repair to happen by an OB.
-
You can have whoever you want at your birth, its YOUR birth. Some people like to give birth in complete privacy, while others want their mom, sisters, cousins, a doula, a photographer, oh and their kids too!
However, We encourage each person you invite to have a specific role in supporting you and your birth goals. Simply consider if you feel ok pooping, being naked, and crying in front of them. Additionally, we strongly believe that the people who are present at your birth should align with your values. There is no room for placing their fears on you in this pinnacle time.
-
Your baby's birth certificate information will be submitted and instructions will be provided on how to obtain the birth certificate. The Newborn Metabolic Screening and Congenital Heart Defect Screening are offered at the first postpartum visit.
We will perform weight checks at every postpartum visit, ensuring adequate weight gain and timely referrals, as necessary.
Resource: https://floridanewbornscreening.com/
-
We do not clamp or cut the cord until you are ready, or unless there is a medical indication to. Many times this does not occur until approx. 2+ hours when we are completing the newborn exam.
-
YES! Full Circle Midwifery believes in making more midwives for our community to have choices in care and ensuring we have midwifery care for our daughters and granddaughters. There are 3 different levels of student midwives; observe, assist, and primary under supervision.
Students in the observe phase are very new to birth or home birth and are there to clean, set up and breakdown, and “watch” the midwife and birth process.
The assist phase of the journey is a bit more hands on. These students are learning to take vitals, chart, use equipment and tools, and the art of midwifery. They will NOT “catch” your baby, repair a tear, assume management of complications, or ever be left alone at your birth. They are primarily there to literally assist the midwife.
The primary under supervision role is very unique. This student is at the very end of their training and is competent in care. They are under supervision and guidance of the midwives at all times but will be acting at the primary midwife. This means “running” penatal visit, completing necessary or desired exams, managing complications, completing all paperwork, and embodying your midwife. They are a midwife already, and are practicing with supervision for their growth, skill development, fine tuning, and your safety.
We will usually have 1 student at a birth. This allows for a well rested team, shared burden of cleaning and equipment care while still keeping your birth team small and intimate. If you prefer NO STUDENTS, this is understandable and will be discussed throughout our care together.
-
Yes! We love doulas. Check out the evidence on doula care. https://evidencebasedbirth.com/the-evidence-for-doulas/
-
Absolutely!
Learning about your cycle:
- Taking Charge of Fertility (the BEST book to get started)
- Basal Body thermometer for temp tracking.
- Inito or Mira are cool tech for tracking your cycle through hormones.
Getting your GUT and nutrition right! There is so much new evidence that the healthy gut affects so much in your life, but especially fertility. The book " The Mind-Gut Connection - by Emeran Mayer” is a great way to start learning. Also, nutrition; this book "Real food for fertility" is the best place to start.
We have some really cool people to follow, and connect with right here in Florida! Reach out to us for more information on your local resources.